Introduction
The OHL is increasingly acknowledged as a crucial element of public health, vital for ensuring the general health and well-being of individuals (Alzahrani et al., 2024). OHL comprises the skills necessary to access, process, and comprehend fundamental oral health information and services, enabling individuals to make well-informed decisions about their oral health (Dickson-Swift, Kenny, Farmer, Gussy, & Larkins, 2014). Also, OHL goes beyond mere literacy, incorporating the ability to navigate the healthcare system, communicate effectively with healthcare providers, and apply preventive and therapeutic measures effectively (Brega et al., 2019). Additionally, low OHL has been linked to poor oral health outcomes, including higher rates of dental caries, periodontal disease, and tooth loss, as well as a diminished quality of life (Adil et al., 2020; Batista, Lawrence, & Mdlrd, 2018). Recognizing and enhancing OHL is essential for reducing health disparities and promoting fairness in oral health care (Ramos-Gomez & Tiwari, 2021).
Research consistently demonstrates that individuals with low OHL are less inclined to participate in preventive dental practices, more prone to having untreated dental issues, and often encounter greater difficulties in accessing dental care services (Lee, Divaris, Baker, Rozier, & Vann, 2012; Ueno, Takeuchi, Oshiro, & Kawaguchi, 2013). Moreover, OHL exhibits a significant relationship with socioeconomic factors, including education level, income, and healthcare resource access (Adil et al., 2020). This correlation emphasizes the necessity of designing targeted interventions to improve OHL among vulnerable populations (Baskaradoss, 2018).
Efforts to improve OHL can take various forms, including educational programs, community-based initiatives, and policy changes that promote health equity (Council, Bo, Youth, Coohat, & Institute of Medicine and National Research Council, 2012; Petersen & Kwan, 2011). Moreover, incorporating oral health education into school curricula, training healthcare providers to communicate more effectively with patients, and developing culturally sensitive educational materials can significantly impact OHL levels (Lawler, Farrell, Fitzgerald, Jones, & Cullen, 2023; Nakre & Harikiran, 2013). Additionally, leveraging digital health tools and resources offers promising avenues for expanding access to oral health information and support (Srivastava, Tangade, & Priyadarshi, 2023). It is crucial to address OHL to achieve better oral health outcomes and narrow the gap in health disparities (Bukhari 2023). By emphasizing education, communication, and accessibility, individuals can be empowered to take charge of their oral health, leading to a better quality of life (Petersen & Yamamoto, 2005).
Defining and Measuring OHL
The OHL plays a important role in self-care and the utilization of oral health services. It determines an individual's aptitude to recognize and follow instructions of oral health, adhere to treatment plans, and engage in preventive behaviors (Kaur, Kandelman, & Potvin, 2019). Moreover, OHL levels have been found to have a positive impact on oral health outcomes, such as reduced incidences of dental caries, periodontal disease, and oral cancer (Ahmed et al., 2021). On the other hand, low levels of OHL have been linked to poorer oral health outcomes, increased disease prevalence, and higher healthcare costs (Baskaradoss, 2018). Furthermore, research indicates that individuals with low OHL are more likely to exhibit poor oral hygiene practices, delay seeking dental care, and experience higher rates of dental anxiety and fear (Badran, Keraa, & Farghaly, 2023; Baskaradoss, 2016; Firmino et al., 2018).
The measurement of OHL is essential for identifying at-risk populations and tailoring interventions to improve health outcomes (Nutbeam & Lloyd, 2021). Multiple tools have been created to evaluate OHL, each employing a distinct methodology and emphasis. The Rapid Estimate of Adult Literacy in Dentistry (REALD-30) is a widely used tool that measures the ability to read and pronounce common dental terms (Lee, Rozier, Lee, Bender, & Ruiz, 2007). Additionally, another notable instrument is the Test of Functional Health Literacy in Dentistry (TOFHLiD), which assesses comprehension and numeracy skills related to oral health (Sabbahi, Lawrence, Limeback, & Rootman, 2009). Moreover, a scoping review by D Dickson-Swift et al. (2014) (Dickson-Swift et al., 2014) highlighted the diversity of OHL measurement tools and underscored the need for standardization in this area to facilitate comparative research and intervention design.
Improving OHL in populations
There is a persistent association between low OHL and negative oral health outcomes. Individuals with insufficient OHL are less inclined to participate in preventative strategies, such as consistent brushing and also the flossing of teeth, and are more susceptible to the development of dental caries and periodontal disease (Geethapriya, Asokan, Kandaswamy, & Shyam, 2020; Northridge, Kumar, & Kaur, 2020). Moreover, they are also less likely to seek timely dental care, resulting in the progression of oral diseases and complications that could have been prevented or mitigated with earlier intervention (Horowitz & Kleinman, 2008; Jones, Lee, & Rozier, 2007). Furthermore, OHL is influenced by various socio-demographic factors, including age, education, income, and ethnicity (Noor, Rani, Zakaria, Yahya, & Sockalingam, 2019). Research indicates that elderly populations and those with lower educational attainment often have lower levels of OHL (Kridaningrat, Soegyanto, & Wimardhani, 2017). Additionally, socioeconomic status also plays a significant role, with disadvantaged groups typically exhibiting poorer OHL (Chaffee, Rodrigues, Kramer, Vítolo, & Feldens, 2017). Blizniuk, Ueno, Zaitsu, and Kawaguchi (2015) (Blizniuk et al., 2015) conducted a study in Belarus and found that individuals with lower socio-demographic status had significantly lower OHL levels, which in turn were associated with poorer oral health behaviors and outcomes.
Certain populations are particularly vulnerable to the effects of low OHL. Indigenous populations and ethnic minorities often exhibit lower levels of OHL, contributing to disparities in oral health outcomes ( ; Valdez et al. 2022) (Divaris, Lee, Baker, & Vann, 2011). Moreover, PParker and Jamieson (2010) (Parker & Jamieson, 2010) explored the associations between OHL and oral health outcomes among Indigenous Australians, finding significant correlations between low literacy levels and poorer health outcomes. These findings highlight the need for targeted interventions to address OHL in vulnerable populations. Improving OHL requires effective communication between dental professionals and patients (Tseng et al., 2021). This includes using plain language, visual aids, and teach-back methods to ensure patient understanding. Additionally, educational interventions, such as workshops and informational materials, can also enhance OHL among patients (Nurash, Kasevayuth, & Intarakamhang, 2020). Guo et al. (2014) (Guo et al., 2014) emphasized the importance of culturally sensitive communication strategies to improve OHL among diverse populations.
Community-based programs aimed at improving OHL have shown promise in addressing disparities in oral health. Moreover, these programs often involve collaborations between healthcare providers, educators, and community organizations to deliver targeted education and resources to underserved populations (Thomas, 2022). Additionally, advocating for policies that support OHL is essential for long-term improvements. This includes integrating oral health education into school curricula, funding community health programs, and promoting public awareness campaigns (Bersell, 2017). Policies that facilitate access to dental care and prioritize preventive services can also contribute to higher levels of OHL (Ramos-Gomez & Tiwari, 2021). NaghibiSistani, Yazdani, Virtanen, Pakdaman, and Murtomaa (2013) highlighted the need for policy initiatives that address the social determinants of health and reduce barriers to oral healthcare (Sistani et al., 2013). This review aims to examine the current state of OHL research, evaluate the effectiveness of different interventions designed to improve OHL, and provide recommendations for future initiatives.
Table 1
Sources and searched strategies information.
Method
Literature Search Strategy
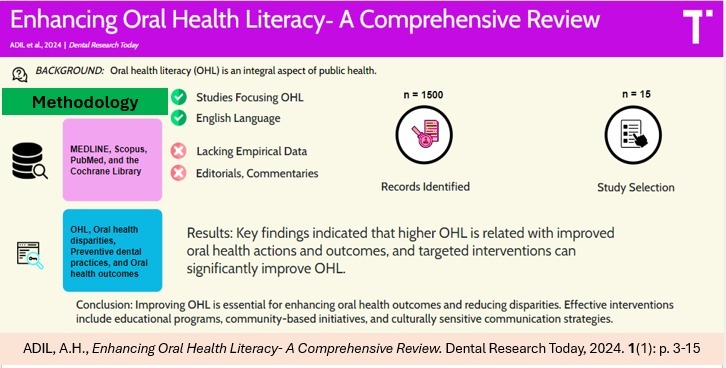
A comprehensive literature search was conducted using several electronic databases, including PubMed, MEDLINE, Scopus, and the Cochrane Library, to identify relevant studies on OHL (Table 1 ). The search strategy was designed to capture a broad range of articles related to OHL, encompassing various aspects such as its definition, measurement, impact on health outcomes, and interventions aimed at improving OHL. The search terms used included combinations of keywords and phrases such as "oral health literacy," "dental health education," "health disparities," "preventive dental practices," "health communication," and "public health." Boolean operators (AND, OR) were used to refine the search and ensure comprehensive coverage of the topic. The search was limited to peer-reviewed articles published in English from 2000 to 2024.
Study Screening
The preliminary search produced a significant quantity of articles. The initial round of screening involved evaluating the titles and abstracts of all identified publications to ascertain their pertinence to the subject of OHL. Articles that did not focus on OHL or those that were not empirical studies, were excluded at this stage. The remaining articles were then subjected to a full-text review.
Inclusion criteria
Studies should focus on OHL by either creating and validating measurement techniques, assessing the effectiveness of OHL interventions, or investigating the connection between OHL and health outcomes. Studies must incorporate empirical data, encompassing quantitative, qualitative, or mixed methodologies. Publication of articles is restricted to peer-reviewed journals. Publication of studies is required to be in the English language.
Exclusion criteria
Studies that did not focus primarily on OHL. Articles that lacked empirical data (e.g., editorials, commentaries, reviews without new data). Publications in languages other than English. Studies with significant methodological limitations that could affect the validity of their findings.
Data Extraction and Synthesis
Data from the included studies were extracted using a standardized data extraction form. The form was designed to capture key information about each study, such as author(s), publication year, country, study design, sample size, population characteristics, data collection techniques, and potential biases, was critically evaluated to provide a clearer understanding of the strengths and limitations of the research. Tools and methods used to assess OHL. Description of any interventions aimed at improving OHL, including their components, duration, and delivery methods. Primary and secondary outcomes were measured, including changes in OHL levels, oral health behaviors, and clinical oral health outcomes. Summary of the main results and conclusions of each study. Each study's design, including sampling methods.
Table 2
Summary of included studies.
Author, Date, and Title | Purpose | Intervention | Sample Characteristics | Measurement of OHL | Findings |
|---|---|---|---|---|---|
(Gong et al., 2007) , "Development and Testing of Test of Functional Health Literacy in Dentistry TOFHLiD" | To assess the reliability as well as precision of the TOFHLiD | Creation of a new measurement tool for OHL | Adults from diverse backgrounds (n=102) | TOFHLiD | While TOFHLiD shows strong convergent validity, its capacity to distinguish between dental and medical health literacy is just moderate. |
(Vann, Lee, Baker, & Divaris, 2010) , "Oral Health Literacy Among Female Caregivers: Impact on Oral Health Outcomes in Early Childhood" | To examine the impact of OHL on children's oral health outcomes | Educational sessions for caregivers | Female caregivers of young children (N=1273) | REALD-30, oral health behaviors | Higher OHL in caregivers leads to better oral health in children |
(Sabbahi et al., 2009), "Development and Evaluation of an Oral Health Literacy Instrument for Adults" | To create and assess an OHL tool specifically designed for adult individuals. | Creation of a new OHL measurement tool | Adults from various socioeconomic backgrounds (n=100) | Oral Health Knowledge Test, OHLI, TOHFLA | OHLI is a useful tool for assessing OHL in adults |
(Jones et al., 2007), "Oral Health Literacy Among Adult Patients Seeking Dental Care" | To assess OHL levels among adult dental patients | Use of REALD instrument to measure OHL levels | Adult dental patients (n=101) | REALD-30 & short interview | Low OHL is associated with poor oral health outcomes |
(Macek et al., 2011), “Knowledge of oral health issues among low-income Baltimore adult: A pilot study” | To record the theoretical understanding of oral health among economically disadvantaged persons in Baltimore. | Community-based educational interventions | Low-income adults (n=100) | BHLOHKP, Face-to-face Interview | OHL includes knowledge of basic concepts. Therefore, oral health literacy affects the ability to communicate |
(Bridges et al., 2014), " The relationship between caregiver functional oral health literacy and child oral health status" | To examine the correlation between the oral health status of Asian children and the OHL of their caregivers. | Community-based | Child/parent dyads recruited from kindergartens in Hong Kong (n=301) | HKREALD-30, HKOHLAT-P & oral examination | There was a correlation between the oral health literacy of the caregiver and the oral health status of their child. |
(Jones, Parker, Mills, Brennan, & Jamieson, 2014), " Development and psychometric validation of a Health Literacy in Dentistry scale (HeLD)" | To develop and authenticate a Health Literacy in Dentistry (HeLD) instrument specifically tailored for the Indigenous Australian population. | Creation and evaluation of the HeLD's validity and reliability. Interventions that promote health in the community | Indigenous Australian population (n=400) | HeLD | The HeLD seems to be a valid and trustworthy tool, and it can be used to find out how well people from rural Indigenous Australia understand oral health. |
(Lee et al., 2022), " Gender differences in the association between oral health literacy and oral health-related quality of life in older adults" | To examine gender differences in OHL and oral health-related quality of life (OHRQoL) among Taiwanese community seniors. | Administration of the Oral Health Literacy Adult Questionnaire (OHL-AQ) Nutritional Assessment—Short Form (MNA-SF) Instrumental Activities of Daily Living Scale (IADL) oral hygiene impact profile (OHIP-14T) | Dwelling older adults (n=216) | OHL-AQ | Significant evidence indicated a correlation between OHL and OHRQoL |
(Holtzman, Atchison, Gironda, Radbod, & Gornbein, 2014), "The association between oral health literacy and failed appointments in adults attending a university-based general dental clinic" | To identify the factors that contribute to patients' lack of attendance at a university dentistry clinic, as well as their oral health literacy level. | Community-based survey on oral health literacy and dental attendance | Adults seeking dental care (n=200) | REALM-D | Missing dental visits can be caused by several circumstances. Low OHL abilities, are associated with missed dentist appointments. |
(Batista et al., 2018), " Oral health literacy and oral health outcomes in an adult population in Brazil " | To examine the link between OHL and dental health outcomes. | Community-based cross-sectional survey | Adult patients (n=248) | OHIP-14 | OHL is linked to oral health status and practices like emergency dental care and may affect quality of life. |
(Parker et al., 2012), " An oral health literacy intervention for Indigenous adults in a rural setting in Australia" | This study explores whether a functional, context-specific OHL intervention improves outcomes. | A randomized controlled trial (RCT) employing a delayed interventional strategy. | Adults aged 18 years and older (n=400) | HeLMS | This study employs a practical, context-specific intervention with Indigenous individuals residing in remote areas. |
(Miller, Lee, Dewalt, & Vann, 2010), " Impact of Caregiver Literacy on Children's Oral Health Outcomes" | To explore children's oral health outcomes that are impacted by the literacy levels of their primary caregivers. | Community-based cross-sectional survey | Caregiver and their children (n-106) | REALD-30 | The prevalence of dental diseases in children is strongly correlated with caregiver OHL. |
(Wong et al., 2012), " Development and validation of Hong Kong Rapid Estimate of Adult Literacy in Dentistry" | To develop and validate an instrument , the Hong Kong Rapid Estimate of Adult Literacy in Dentistry | Creation of a new measurement tool for OHL | Parents of pediatric dental patients (n=200) | HKREALD-30 | Initial testing of HKREALD-30 indicates its validity and reliability for evaluating oral health literacy among Chinese individuals in Hong Kong. |
(Gironda, Der-Martirosian, Messadi, Holtzman, & Atchison, 2013), " A brief 20-item dental/medical health literacy screen" | To present a concise 20-item assessment tool for evaluating the level of dental/medical health literacy in adult dental patients. | Community-based cross-sectional survey | Adult patients (n=200) | REALMD-20 | The REALMD-20 is a rapid assessment instrument designed for professionals to detect low levels of dental/medical health literacy in adult patients who are seeking treatment in clinics. |
(Sistani et al., 2013), " Oral health literacy and information sources among adults in Tehran, Iran" | To introduce a short 20-item screener to assess adult dentistry patients' low dental/medical health literacy. | Community-based cross-sectional survey | Adults in Tehran, Iran (n=1031) | Oral Health Literacy Adults Questionnaire (OHL-AQ) | Iranian adults had a low average degree of oral health knowledge. Disseminating evidence-based oral health care information through multiple channels, including TV/radio, dentists, and other health professionals, can improve the public's understanding of oral health. |
(Adil et al., 2020) “Assessment of Parents’ Oral Health Literacy and Its Association with Caries Experience of Their Preschool Children” | To evaluate the level of OHL among parents and its correlation with the occurrence of tooth decay in their preschool children who have attended the Hospital in Kota Bharu, Kelantan, Malaysia. | Community-based cross-sectional survey | Parents of preschool children (n=230) | OHLI-M | There is a strong correlation between the OHL of parents and the decayed, missing, and filled teeth (dmft) score of their preschool children. |
The extracted data were then synthesized to provide a comprehensive overview of the current state of research on OHL. This synthesis involved identifying common themes and patterns across studies, as well as noting any significant differences or gaps in the literature. Where possible, quantitative data were pooled to provide aggregate estimates of the impact of OHL interventions.
Results
Study Selection
A total of 1500 articles were identified during the preliminary literature search. Following the elimination of 1200 duplicate articles, 300 distinct articles were evaluated based on their title and abstract. Out of these, 85 articles were considered relevant and chosen for a comprehensive review of their full content. After conducting a comprehensive assessment of the whole texts, a total of 15 studies were found to meet the specific criteria for inclusion and were therefore included in the final review (Figure 1, Prisma flow chart).
Reasons for Exclusion
Out of the 85 full-text articles reviewed, 70 were excluded for the following reasons: 30 articles did not focus primarily on OHL. 20 articles lacked empirical data. 10 articles were not published in peer-reviewed journals. 10 articles had significant methodological limitations.
Included Studies
The final 15 studies encompassed a diverse array of subjects pertaining to OHL, such as the creation and validation of assessment instruments, the assessment of educational and community-based interventions, and the analysis of the correlation between OHL and oral health outcomes. The studies were conducted in various countries and included diverse populations, providing a comprehensive overview of the global state of research on OHL (Table 2 ).
Discussion
The OHL is a fundamental aspect of public health that significantly influences individuals' ability to manage their oral health effectively (Dieng et al. 2020). This review aims to provide a comprehensive understanding of OHL by examining various studies. Moreover, it highlights the importance of OHL, and discuss the interventions designed to improve it. Although the studies included in this review span diverse populations and employ various methodologies to measure and enhance OHL. The findings of this review underscore the importance of OHL in shaping oral health behaviors and outcomes. Furthermore, the development and validation of various OHL measurement instruments have provided researchers and clinicians with valuable tools to assess and address literacy levels in diverse populations.
Definition and Measurement of OHL
The OHL involves a variety of abilities, such as the capacity to comprehend, interpret, and apply oral health information (Bridges et al. 2014a). Additionally, it encompasses the task of navigation through the healthcare system and efficiently engaging with healthcare providers (Dickson-Swift et al., 2014). However, these abilities are essential for making well-informed choices regarding oral health and executing preventative and therapeutic actions (Petersen 2009). Furthermore, the low OHL level has been linked to negative oral health outcomes, including increased prevalence of periodontal disease, dental caries, and tooth loss, as well as a worse quality of life (Firmino et al., 2017). Similarly, it is crucial to comprehend and enhance OHL in order to decrease health inequalities and advocate for fairness in oral healthcare (Horowitz, Kleinman, Atchison, Weintraub, & Rozier, 2020).
Accurate measurement of OHL is critical for assessing the extent of the problem and evaluating the effectiveness of interventions (Duell, Wright, Renzaho, & Bhattacharya, 2015). Various tools have been developed to measure OHL, each with its strengths and limitations. Moreover, these tools offer valuable insights into an individual's reading skills, comprehension capabilities, and overall understanding of oral health-related information. Despite the availability of these measurement tools, challenges remain in terms of a standardized approach to evaluating OHL across different settings and populations. Furthermore, tailoring measurement strategies to address cultural and language differences is crucial to ensure validity and relevance.Gong et al. (2007) developed and tested the TOFHLiD, which has been validated as a reliable tool for measuring OHL (Gong et al., 2007). This assessment evaluates persons' aptitude in comprehending and utilizing verbal health-related information, which is crucial for properly managing their oral health.
Similarly, the REALD has been widely used to measure OHL.Jones et al. (2007) used the REALD-30 instrument to assess OHL levels among adult dental patients. Their findings indicated that there was an association between low OHL and poor oral health outcomes, underscoring the importance of improving OHL to enhance oral health (Jones et al., 2007). Further,Sabbahi et al. (2009) developed and evaluated an OHL instrument for adults, known as the Oral Health Literacy Instrument (OHLI). This tool has been shown to be useful for assessing OHL in various populations and provides valuable understanding into the association between OHL and oral health behaviors (Sabbahi et al., 2009). Additionally, the study by Jones et al. (2013) successfully developed and validated the HeLD scale for Indigenous Australians. Conducted with 400 participants from rural Indigenous communities, the research assessed the validity and reliability of the HeLD tool through community-based interventions. The findings confirmed that the HeLD is a reliable and valid tool for measuring OHL in this population, providing a valuable resource for understanding and improving oral health literacy among Indigenous Australians.
In their study,Wong et al. (2012) created and verified the Hong Kong HKREALD-30 as a tool for assessing OHL. Moreover, the study, which involved surveying 200 parents of pediatric dental patients, provided evidence that the HKREALD-30 is a reliable and valid tool for assessing OHL in Chinese adults residing in Hong Kong (Wong et al., 2012). Furthermore, this instrument is a valuable resource for evaluating and enhancing OHL in this specific group of people, demonstrating its potential for wider use in similar situations.
Impact of OHL on Health Outcomes
Numerous studies have demonstrated a strong relationship between OHL and oral health outcomes ( ; Mialhe et al. 2022) (Baskaradoss, 2018; Kanupuru, Fareed, & Sudhir, 2015; Kridaningrat et al., 2017; Navabi, Shahravan, Behnood, & Hashemipour, 2020). Moreover, persons with higher OHL are more liable to engage in preventive action, follow treatment recommendations from healthcare professionals, and maintain better overall oral hygiene (Ramos-Gomez & Tiwari, 2021). Conversely, those with limited OHL often struggle to comprehend health information and are more susceptible to misinformation, leading to adverse health outcomes such as delayed care seeking and increased health-related anxiety (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011). For example,Vann et al. (2010) examined the impact of OHL on children's oral health outcomes by assessing the OHL of female caregivers using the REALD-30 instrument. They found that higher OHL in caregivers is related with better oral health outcome in children (Vann Jr et al. 2010). This study emphasizes the significance of directing OHL treatments towards caregivers in order to enhance children's oral health. Similarly, Macek et al. (2010) assessed the relationship between OHL and dental care utilization in adults from Baltimore, Maryland, using the BHLOHKP instrument. The OHL includes conceptual knowledge. Communication is affected by oral health literacy. Furthermore, practitioners should consider low conceptual knowledge when discussing oral health with low-income and minority patients (Macek et al., 2011). This study emphasizes that if oral hygiene education messages may be ignored the health promotion may suffer.
The research conducted by Bridges et al. (2013) emphasizes the substantial correlation between the OHL of caregivers and the oral health status of children. In addition, a study was carried out in Hong Kong involving 301 child/parent pairs from kindergartens. The researchers utilized the HKREALD-30 and HKOHLAT-P tools to assess reading levels and discovered that children with caregivers who had greater literacy levels had improved oral health (Bridges et al. 2014b). Similarly, the study conducted byMiller et al. (2010) highlights the significant impact of caregiver literacy on the oral health results of children. The study included a cross-sectional survey involving 106 pairs of caregivers and children. In addition, the caregiver's OHL was assessed using the REALD-30. The results demonstrated a notable correlation between higher caregiver OHL and a reduced prevalence of dental issues in children. These findings highlight the significance of improving caregiver literacy as a primary approach to enhance children's oral health (Miller et al., 2010). Additionally, it indicates that focused educational interventions for caregivers have the potential to greatly decrease dental disease rates in children.
Adil et al. (2020) investigated the association between parents OHL and their preschoolers' caries experiences. Using the OHLI to assess OHL, cross-sectional survey was carried out with 230 parents at Hospital HUSM in Kota Bharu, Kelantan. The results demonstrated a strong correlation between parents with greater OHL and children with lower dmft scores (Adil et al., 2020). Moreover, this finding underscores the importance of focused educational programs aimed at enhancing parental OHL in order to decrease dental caries in preschool-aged children. Similarly, the link between OHL and dental health outcomes in a Brazilian adult population was investigated by Batista et al. (2018). The study used the OHIP-14 to assess quality of life in relation to oral health in a cross-sectional survey of 248 adult patients conducted in the community. According to the results, a higher OHL is linked to better oral health, which in turn leads to better oral health practices, including less need for emergency dental treatment, and an overall better quality of life (Batista et al., 2018). Furthermore, it is crucial to improve OHL in order to improve adults' dental health and overall health.
Barriers to Improving OHL
Despite the awareness of the significance of OHL, several barriers persist in effectively addressing it within the healthcare system (Tseng et al., 2021). Time constraints during patient consultations often limit the opportunities for providers to engage in educational dialogue (Joseph-Williams, Edwards, & A, 2014). Additionally, systemic issues such as inadequate resources, lack of OHL training among healthcare professionals, and the social stigma associated with low literacy further complicate efforts to enhance OHL (Farmanova, Bonneville, & Bouchard, 2018). Moreover, cultural and language differences can also act as significant barriers (Shaw, Huebner, Armin, Orzech, & Vivian, 2009). Many educational materials and resources are not culturally sensitive or available in multiple languages, which can alienate non-English speaking populations from receiving essential health information (Gao & Mcgrath, 2011). Furthermore, patients from minority backgrounds may experience distrust towards healthcare systems, which can hinder their engagement and willingness to seek help or education (Hong, Yi, Johnson, & Adamek, 2018).
Addressing these barriers requires a multifaceted approach. Healthcare systems must facilitate environments where providers have sufficient time and resources to engage with patients effectively (Khorasani et al., 2020). Moreover, the development of culturally relevant educational materials in various languages can help bridge existing gaps and enhance OHL among diverse populations (Muller, Bilich, & Jones, 2024). Several studies have identified barriers to improving OHL and accessing dental care (Calvasina, Lawrence, Hoffman-Goetz, & Norman, 2016; Lawler et al., 2023; Muller, 2016; Sistani, Virtanen, Yazdani, & Murtomaa, 2017). For example,Holtzman et al. (2014) evaluated OHL and missed dental appointments in university-based general dentistry clinic adults. According to a community-based survey and the REALM-D with 200 adult patients, poor OHL was substantially associated with more missed dental appointments (Miller et al., 2010). This shows that increasing OHL could minimize missed appointments, emphasizing the need for educational programs to increase patient attendance and oral health outcomes. Furthermore,Gironda et al. (2013) developed a simple 20-item screener (REALMD-20) to assess adult dentistry patients' dental and medical health literacy. A cross-sectional study of 200 adult patients showed that the REALMD-20 can quickly and accurately identify low health literacy patients (Gironda et al., 2013). Similarly, this tool can improve patient outcomes by providing low-literate patients with the support and instruction they need to manage their dental health.
Interventions to Improve OHL
Interventions targeting OHL have shown promising results in improving patient understanding and engagement in their oral health (Ju et al., 2017; Kaper, Sixsmith, Reijneveld, & Winter, 2021; Parker et al., 2012). Moreover, educational programs aimed at enhancing OHL can significantly increase individuals' knowledge about oral health and empower them to make informed decisions regarding their oral care (Muller, 2016). These interventions can take various forms, including community workshops, targeted informational brochures, and personalized counseling sessions ( ; Ebrahimi and Farokhi 2022) (Jacobs, Lou, Ownby, & Caballero, 2016). Furthermore, efforts to improve OHL can take various forms, including educational programs, community-based initiatives, and policy changes that promote health equity (Mathias et al., 2023). For example,Holtzman et al. (2014) evaluated OHL and missed dental appointments in university-based dental clinic adults. A community-based survey and the REALM-D with 200 adult patients indicated that poorer OHL was substantially associated with more missed dental appointments (Holtzman et al., 2014). This suggests that focused educational programs to enhance OHL may improve dental attendance and oral health outcomes by reducing appointment non-attendance.
The research conducted by NaghibiSistani et al. (2013) evaluated OHL among adults residing in Tehran, Iran. The study employed a community-based cross-sectional survey involving 1031 participants. The study employed the OHL-AQ to determine that Iranian people had an average level of OHL. Furthermore, the results indicate that spreading evidence-based oral health information through different channels, such as dentists, radio/TV, and other health professionals, has the potential to greatly improve public OHL (Sistani et al., 2013). This highlights the need for multi-channel educational strategies to improve oral health outcomes in the population. Similarly,Parker et al. (2012) tested a functional, context-specific OHL intervention for Indigenous individuals in rural Australia. In this delayed intervention randomized controlled trial, 400 Indigenous persons aged 18 and older participated. Participants' OHL improved significantly after the context-specific intervention, according to the HeLMS (Parker et al., 2012). This suggests that culturally sensitive therapies can improve oral health in distant Indigenous groups. Furthermore,Lee et al. (2022) examined gender differences in OHL and OHRQoL in older Taiwanese individuals. The study used the OHL-AQ, MNA-SF, IADL, and OHIP-14T on 216 older persons. Additionally, OHL and OHRQoL were significantly correlated, with gender differences (Lee et al., 2022). This emphasizes the need for gender-specific interventions to improve OHL and older adults' quality of life.
The Role of Technology in Enhancing OHL
The digital age has introduced innovative methods for improving OHL through technology (Jagde et al. 2021). Online platforms, interactive applications, and webinars offer accessible resources that can equip individuals with essential oral health knowledge (Dahiya, Khanna, Dogra, & Jaglan, 2024). Research has highlighted the potential of using mobile applications to promote oral health literacy, providing users with easy access to valuable information tailored to their needs, such as appointment reminders, oral hygiene tips, and dietary guidelines (Tiffany, Blasi, Catz, & Mcclure, 2018). Moreover, e-learning modules have shown effectiveness in training healthcare providers to communicate relevant health information effectively (Lawn, Zhi, & Morello, 2017). Online platforms offer flexibility for professionals seeking to enhance their communication strategies and improve their understanding of OHL-related issues (Claflin et al., 2022). However, while technology can serve as a powerful tool for improving OHL, it is essential to consider the digital divide (Bayazıt & Bayazit, 2023). Although, access to technology varies significantly among different populations, particularly those from lower socio-economic backgrounds. Furthermore, ensuring that all individuals can access technological resources is crucial for developing equitable OHL interventions (Sharma, Mohanty, Balappanavar, Chahar, & Rijhwani, 2022).
Future Directions in Oral Health Literacy Research
Ongoing and future research endeavors should focus on several key areas to advance the understanding of OHL and its implications. First, it is essential to continue investigating how OHL affects various population groups, including children, older adults, and marginalized communities. Understanding these dynamics can help tailor interventions to specific groups, thereby enhancing their efficacy. Moreover, research should also explore the integration of OHL assessments into routine dental practices. Developing standardized standards for evaluating OHL in patients can help identify those who are more likely to have negative health effects at an early stage. Furthermore, doing an analysis of the enduring consequences of educational interventions will yield useful insights into their long-lasting viability and efficacy. Furthermore, interdisciplinary collaborations between oral health professionals, public health educators, and researchers can foster innovations in OHL strategies and interventions. By bringing together diverse perspectives and expertise, these collaborations can lead to the development of holistic approaches that encompass various determinants of health and improve OHL comprehensively. However, there is a pressing need to advocate for policies that prioritize OHL as a fundamental component of healthcare. Policymakers should recognize the importance of OHL in addressing health disparities and invest in strategies that facilitate access to education and resources for all individuals.
Limitations of the Review
Although this review offers a comprehensive analysis of the current research on OHL, it does have a few limitations. The review is restricted to papers published in English language; potentially disregarding pertinent material available in other languages. In addition, the review specifically examines cross-sectional research, which offer useful insights on the correlation between OHL and oral health outcomes but are unable to establish causation. Subsequent investigations should incorporate longitudinal studies to evaluate the enduring effects of OHL treatments.
Conclusion
We acknowledge that our review technique may not have included all the research that utilize OHL to inform the development of interventions and evaluate effects in community populations. However, the lack of intervention trials that accurately demonstrate the 'skills-directed' techniques key to the OHL idea, along with the ongoing difficulty in measuring these abilities, should be a source of caution. Although there has been progress in comprehending and encouraging OHL, there is still a pressing requirement for more focused study and the creation of interventions.
It is essential to focus on OHL in order to promote improved oral health results and decrease inequalities in health. Through the prioritization of education, communication, and accessibility, we may enable individuals to assume authority for their oral health and enhance their overall quality of life. The research analyzed in this review emphasize the significance of OHL in promoting oral health and demonstrate the efficacy of different interventions in enhancing OHL. Subsequent studies should prioritize the creation and assessment of novel approaches to improve OHL, specifically targeting disadvantaged groups. Additionally, efforts should be made to enforce policy modifications that foster equal access to healthcare.